常见病如何选题?看美国在研的170项青光眼基金,你就会脑洞大开!(2024)
时间:2024-10-23 14:01:50 热度:37.1℃ 作者:网络
很多朋友问“常见病如何选题”?
今天分享的青光眼就是罕见病。显然,
-
诊断方面可以从“新技术引领下的诊断进步”方面做,如下面的OCT;
-
治疗方面,同样可以借助最新的技术进步,如细胞疗法、免疫疗法、基因疗法等,文末的课题则研究了青光眼中的细胞替代疗法。
我们一起看Amber给我们解读的具体内容。
青光眼(Glaucoma)是一种由于眼内压增高或眼部压力异常引起的视神经损伤,可能导致视力丧失甚至失明。它是一种慢性进展性的眼病,是全球范围内不可逆失明的主要原因之一。
尽管近年来在青光眼的诊断和治疗方面取得了显著进展,但仍存在一些重要而未解决的临床问题:
-
早期诊断困难:青光眼的早期通常没有明显症状,很多患者在中晚期才被发现。虽然眼压测量、视野测试和视神经检查等工具可以帮助诊断青光眼,但还缺乏有效的广泛筛查方法,尤其是对于高风险人群。
-
治疗的个体化和持续性管理:现有的治疗方法(如眼药水、激光治疗和手术)主要集中在降低眼内压,延缓视神经损伤的进展。然而,治疗的效果因人而异,且部分患者对现有疗法响应不佳。如何开发个体化的治疗方案并确保患者的长期依从性仍是临床挑战。
-
长期治疗依从性:青光眼通常需要终身治疗,但患者的依从性是个挑战。眼药水等治疗方法需要每天使用,部分患者可能难以坚持,尤其是在早期没有症状时。寻找更便捷、长期有效的治疗手段,如植入性药物释放装置,可能是未来研究的方向。
-
视神经损伤的不可逆性:青光眼导致的视神经损伤是不可逆的,如何有效保护视神经并预防进一步的损伤是研究的重点。目前,科学家正在研究神经保护和再生技术,但仍处于早期阶段。
-
全球负担:在许多低收入和中等收入国家,青光眼的早期筛查和治疗资源有限。全球范围内需要提高对青光眼的意识,增强早期干预,减少失明率。
青光眼的治疗和管理仍然面临诸多挑战,尽管医学界在控制眼压和保护视神经方面取得了显著进展,如何实现早期诊断和有效保护视力仍然是需要继续解决的难题。未来的研究需要着眼于更好地理解青光眼的发病机制、开发新的治疗策略,以及改善患者的生活质量。
我们仅对美国国立卫生研究院(NIH)资助的在研青光眼相关项目进行梳理,希望给同仁们的选题思路提供一点启发。
2024年,以“Glaucoma”为检索词、在题目中进行检索,美国NIH针对青光眼的在研有170项。
一,谁获得了这些研究?
1,在研青光眼基金最多的PI
-
UNIVERSITY OF MICHIGAN AT ANN ARBOR 的 NEWMAN-CASEY, PAULA ANNE
-
NEW YORK UNIVERSITY SCHOOL OF MEDICINE 的 WOLLSTEIN, GADI
-
ICAHN SCHOOL OF MEDICINE AT MOUNT SINAI 的 PASQUALE, LOUIS ROBERT
-
INDIANA UNIVERSITY INDIANAPOLIS 的 MEYER, JASON STEPHEN
-
UNIVERSITY OF PENNSYLVANIA 的 O'BRIEN, JOAN M
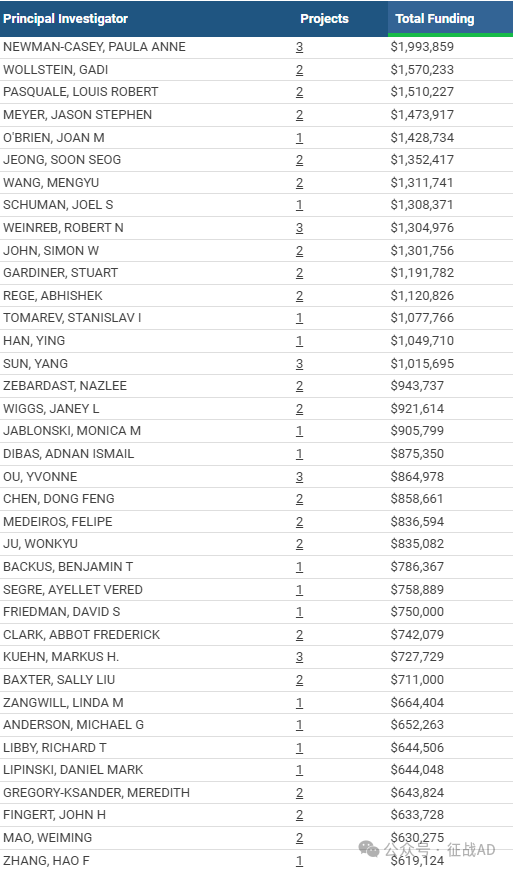
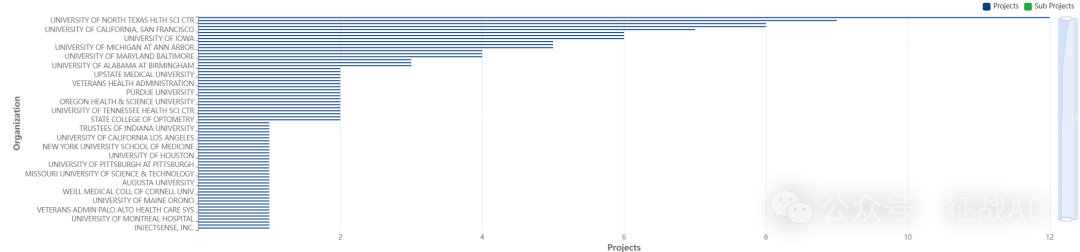
2,青光眼基金最多的研究机构
-
加州大学圣地亚哥分校
-
马萨诸塞州眼耳医院
-
SCHEPENS 眼科研究所
-
加州大学旧金山分校
-
北德克萨斯大学健康科学中心等
二,青光眼研究热点是什么?
青光眼研究领域总览(根据关键词)

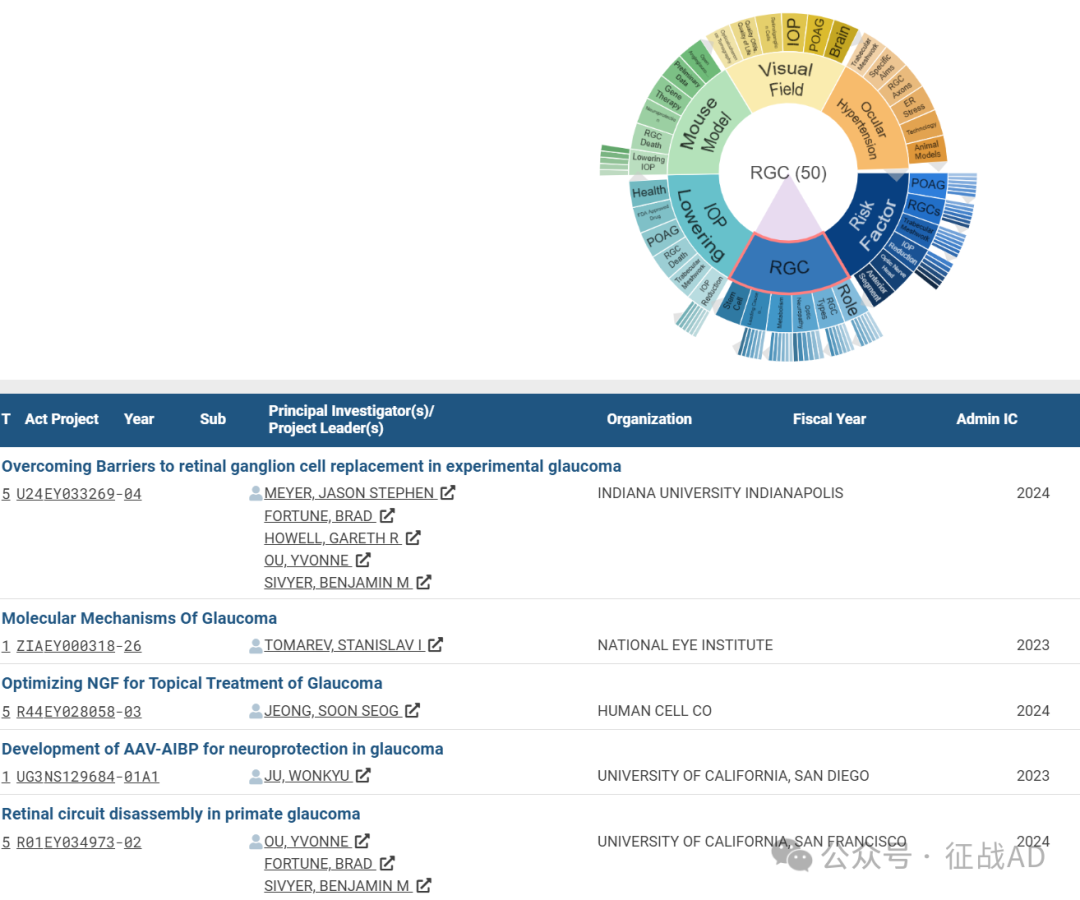
A,关于视网膜神经节细胞(RGC)的研究项目最多
有 50 项在研基金涉及到了视网膜神经节细胞,关注最多的方面包括角色(Role)、视网膜神经节细胞类型(RGC Types)、视神经病变(Optic Neuropathy)、代谢(Metabolism)、不可逆失明的主要原因(Leading Cause of Irreversible blindness)、干细胞(Stem Cell)等研究。
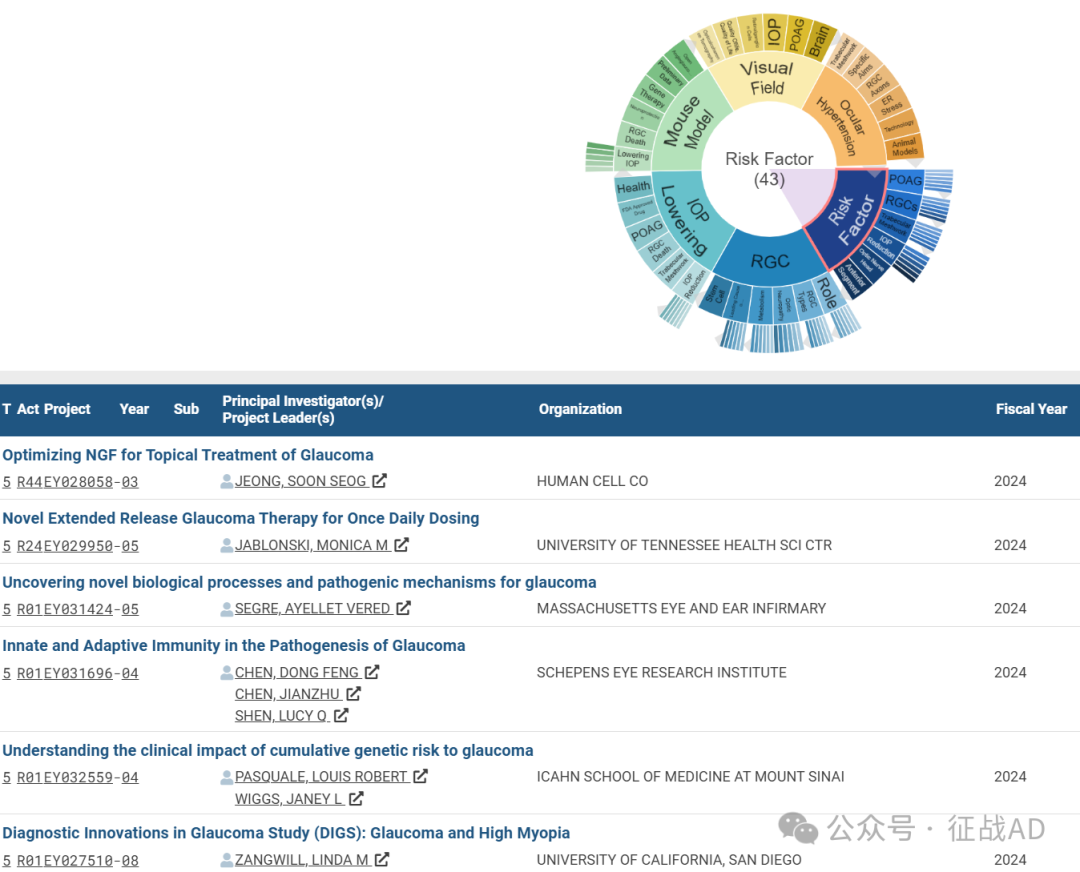
B,关于风险因素(Risk Factor)的研究项目
有 43 项在研基金涉及到了风险因素,关注最多的方面包括POAG、RGCs、小梁网(Trabecular Meshwork)、眼压降低(IOP Reduction)、视神经乳头(Optic Nerve Head)、眼前节(Anterior Segment)等研究。
C,关于眼压降低(IOP Lowering)的研究项目
有 42 项在研基金涉及到了眼压降低,关注最多的方面包括健康(Health)、FDA批准药物(FDA Approved Drug)、POAG、RGC死亡(RGC Death)、小梁网(Trabecular Meshwork)、眼压降低(IOP Reduction)等研究。
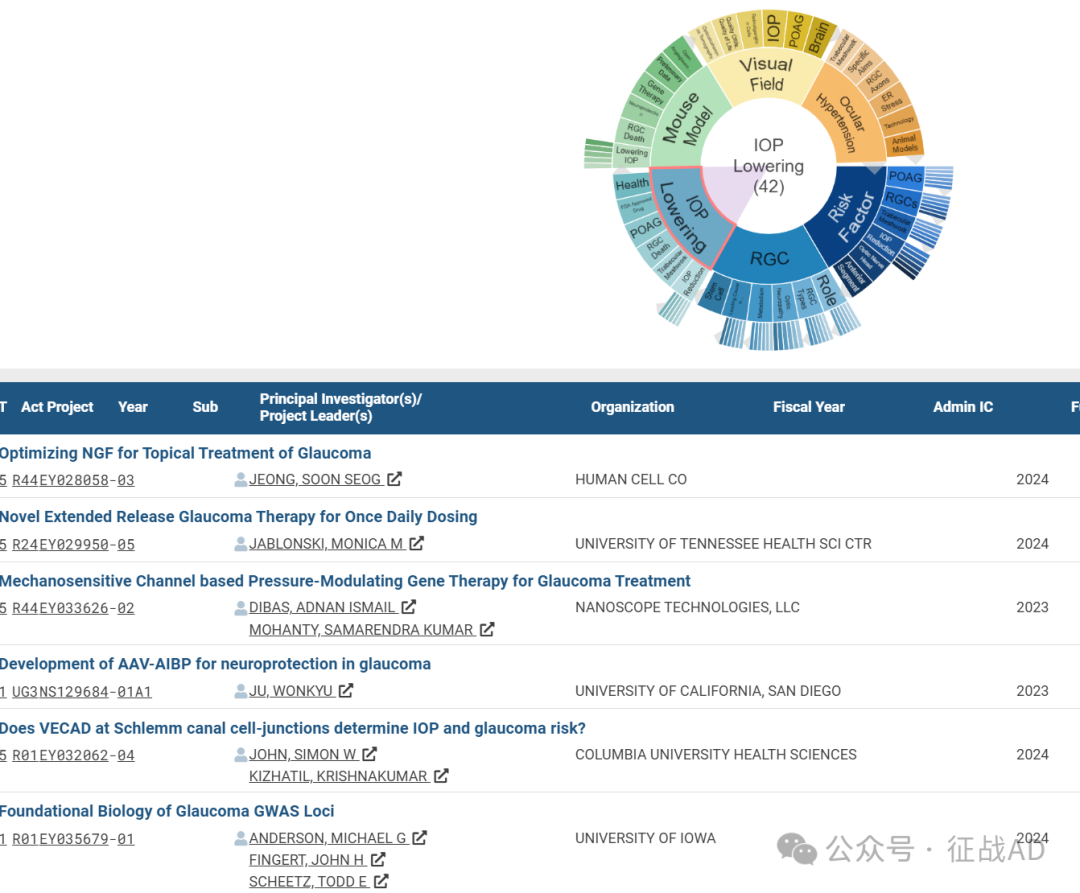
其他青光眼研究大的方向还包括小鼠模型(Mouse Model)、视野(Visual Field)、眼压升高(Ocular Hypertension)等。
三,借鉴与突破
我们也分享在青光眼领域的几项课题摘要,希望对同仁们有所启发。
A,Overcoming Barriers to retinal ganglion cell replacement in experimental glaucoma
Our translation-enabling approach builds on a very well-established, thoroughly characterized and validated experimental glaucoma (EG) model. This affords our study the distinct advantage of conducting each of the proposed hypothesis-driven experiments within the framework of a reliable model of RGC degeneration that closely recapitulates the anatomical changes and pathophysiological processes observed in human glaucoma. Moreover, our preliminary results establish the feasibility of our approach, demonstrating that we have already achieved successful transplantation of human induced pluripotent stem cell (iPSC)-derived RGCs into the EG retina, while also characterizing major barriers that require targeted solutions. Hence, we propose to employ a series of manipulations to both donor RGCs and the recipient EG retina in order to overcome the existing barriers to RGC replacement and thus make a giant leap forward toward realization of the audacious goal to restore vision in persons blinded by glaucoma or other optic neuropathies.
Each of our Aims is soundly based on existing knowledge of the relevant biology and will lead to meaningful enhancement of donor RGC survival, integration, and function in the glaucomatous EG retina. We will utilize rigorous quantitative electrophysiological and anatomical assessments for testing the hypothesis at the core of each Aim. Aim 1 will target neuroinflammation to improve the long-term survival of transplanted RGCs. We will create hypoimmunogenic iPSCs and manipulate the host retinal environment using systemic immunosuppressive agents or inhibition of microglial activation. Aim 2 will augment donor cell survival and integration through modulation of cellular age, with host retinal glia experimentally induced to an immature state through cellular rejuvenation. Aim 3 will enhance the connectivity and axon outgrowth of donor RGCs in the retina. Donor RGCs will be edited to express hM3Dq DREADD receptors for chemogenetic stimulation and mTOR activators. Thrombospondin will be overexpressed in host retinal astrocytes and donor RGCs, leveraging astrocyte-derived factors that promote axonal outgrowth and synaptogenesis.
B, Novel Glaucoma Diagnostics for Structure and Function.
In this proposal, we build on our long-standing contribution to ocular imaging and propose novel and sensitive means to detect glaucoma and identify and predict progression that are optimized to the various stages of disease severity.
We will use advanced signal and image processing and image analysis techniques for OCT, a leading ocular imaging technology, to improve and harmonize images agnostic to OCT acquisition device. Commonly used parameters provided by the technologies and newly developed parameters found to have good diagnostic potential will be analyzed across the entire disease severity spectrum to identify optimal metrics for each stage of the disease.
We will use state-of-the-art machine learning methods, including deep learning and diffusion modelling analysis approaches, to identify structural features embedded within OCT images that are associated with glaucoma and its progression without any a priori assumptions. This will provide novel insight into structural information and has shown very encouraging results to date.
We will use recently developed analytical techniques including multidimensional information compression analysis (MICA) utilizing cluster structure function, a compression-based criterion function for optimizing visualization and clustering via low-dimensional embeddings of the OCT images as well as enhanced machine and deep learning models incorporating clinical features with OCT and visual fields to significantly improve glaucoma detection and the identification of progression and prediction of future disease progression. This program will advance the use of structural, functional, and other clinical information to produce a significant impact on the clinical management of subjects with glaucoma.


